How human-centred design can be used in end-of-life care
End-of-life care is a discipline that covers all aspects of humanity, helping people at the end of their life to live as well as possible until they die. Some people have a clear view of how they wished to be cared for at the end of their life, many do not. However care and treatment at the end of life is complicated, making people’s wishes more difficult to deliver. While the UK leads the world with clinical practices, with decades of pioneering research and robust foundation of evidence, the field as a whole can often lag behind in terms of adopting innovative practices and technology compared to other clinical fields.
Human-centred design offers a powerful way to improve healthcare. By identifying the human needs of people, and working with them, design can take a multifaceted approach to solving some of the most complex problems. Of all the areas in healthcare that would greatly benefit from design innovation and a human-centred approach, it is end-of-life care. Simply put, the needs are the most human: it demands a holistic approach to support clinical treatments, along with emotional and social support for the patient and family, while always focusing on the relationships of everyone involved. We understand there is an appetite by the global palliative medicine profession to set out and build a positive vision that tackles 21st century challenges, expressed with a flexibility to experiment, openness to collaborate and desire for change. Human-centred design is an effective tool to support the palliative medicine profession in its goals.
Applying design in healthcare at the Helix Centre
The Helix Centre is a healthcare innovation studio, embedded inside St Mary’s Hospital in London, led by Professor the Lord Ara Darzi at Imperial College London. Established in 2014 as a collaboration between Imperial College London and the Royal College of Art, we are a team of designers, technologists and clinicians tackling some of the most pressing challenges in healthcare.
We believe design and technology will play a natural and fundamental part in defining the next decades of end-of-life care. It is increasingly accepted that technology will continue to integrate into everybody’s daily lives, and global healthcare systems as a whole are embracing technology at the heart of their work.

The Helix Centre, during one of our design workshops
In our studio, we employ various processes to rapidly dissect a problem, highlight areas of opportunity and prototype solutions. We collaborate internally alongside other subject matter experts to explore opportunity areas from their unique perspectives. We consider everything from a user’s motivations and behaviours, to the viability of potential business models, to the feasibility of technological execution. We co-create solutions with frontline healthcare professionals, academics and the general public.
We have a dedicated team who work on a number of end-of-life care projects. Our aim is to research and design innovative solutions that improve the quality of life for people - young and old - living with life-limiting conditions or are at the end of their life. We are committed to alleviating suffering for dying people, empowering them to live their life to the fullest and to transform the support and experience their families and carers receive as well as professionals and health systems alike. We have been developing three active areas of work that broadly address end-of-life care in the hospital, the home and the hospice.
Enabling conversations in emergency care settings
To understand the current problems for end of life care, it is important to begin in the place where death occurs the most: the hospital. Nearly half of all deaths in England occur in hospitals (223,007 out of 469,975 in 2014), with 69-82% of those who die needing palliative care. Despite this large proportion of people dying in hospital, only 3% actually want to.
Talking about death in a hospital can be incredibly difficult. The curative setting builds an expectation with patients that they are going to get better, and receive long-prolonging treatment at all costs. Many feel that the responsibility for discussions around palliative or end of life treatments should come from clinicians.
End-of-life care in this context is often delivered last minute, following an acute episode that places extraordinary strain on patients, families and clinicians to have meaningful conversations in a short time frame, about the possibility of dying. These conversations at the end of life often form around decisions not to resuscitate the patient. Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) forms are used in these instances, and are widespread having been put in place for 94% of patients’ notes at the time of death.
DNACPR forms are used to make specific clinical decisions for an individual if their heart or lungs stop working, but their use has been linked to many problems. The forms vary within NHS Trusts and community settings, meaning that some people have multiple forms to suit each setting; and there are cases of DNACPR forms having been created without the knowledge of the person or their loved ones. Having difficult conversations about declining health is a vitally important part of how we care for people with life-threatening conditions.
To help improve the way in which end-of-life care is delivered in hospitals - and in collaboration with the Resuscitation Council and a working group of other 30 national organisations - we have helped redesign the way in which difficult conversations about life-sustaining treatments are conducted and recorded with a new form and process called ReSPECT. ReSPECT is a clinician-led process that brings the patient to the centre of the emergency care decisions.
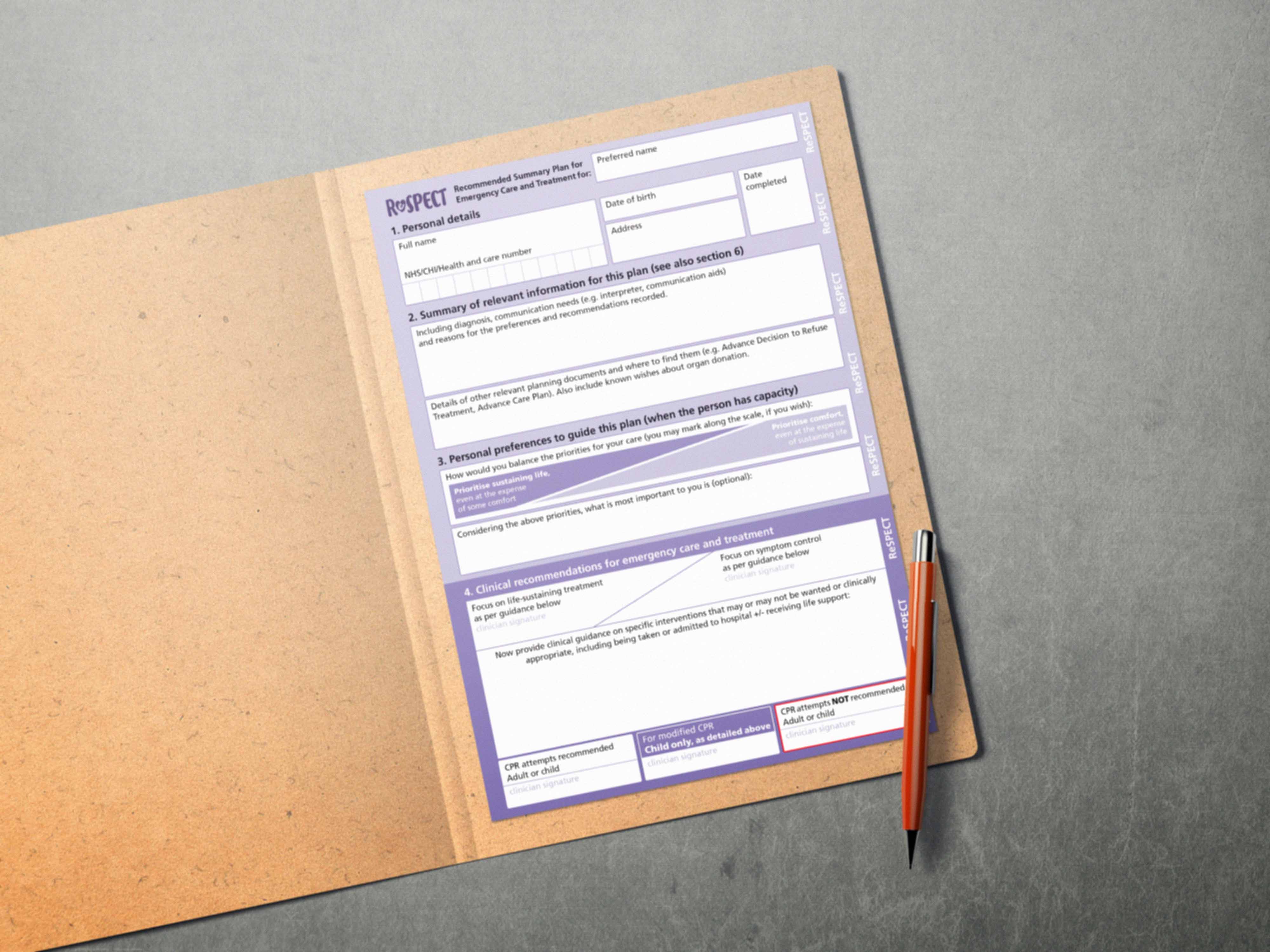
The ReSPECT form
At the centre of the ReSPECT process is a form which is designed to guide a conversation between healthcare professionals and the patient. It features a graphic device used to demonstrate that there is often a compromise between sustaining life and providing comfort and dignity. We helped to clarify this process for patients, to make it accessible and easy to understand.
One of the biggest challenges in introducing a new procedure to the healthcare sector is educating and supporting the people that need to use it. Indeed, clinicians in general get very little training in holding ‘difficult conversations’ specifically and end-of-life care in general. So in response, Helix created a prototype web app to provide accessible training and support to clinicians using the ReSPECT process. This prototype was then developed further, and delivered to professional audiences in a collaboration between Helix Centre Clinical Research Fellow Dr. Gehan Soosaipillai, UCLPartners and Tom Stables Associates. This new digital tool enables healthcare professionals learn about the new process with interactive training scenarios and discussion tips.
To date, the new ReSPECT process has been implemented in over 130 sites across the UK and Ireland, and is being evaluated by Warwick University.
Making advance care planning more personal and better connected
As the population ages, and medical knowledge advances, the importance of giving people more choice and control over their care has never been greater. Getting people to fill in an advance care plan (ACP) has been shown to be highly effective in aligning healthcare with patient's wishes, reducing hospital bed days in over-65s, and moving deaths from the hospital to the community.
However, filling in ACPs is currently human resource intensive and is putting a strain on GPs, palliative care teams, charities and volunteers. The result is that not enough plans are ever being completed. We understand that carefully structured conversations that explore patient's values, not forms, will be the key to increasing uptake of advance care plans. While they are predominantly person-to-person or form-based, the service cannot scale.
We have successfully created the first spin-out venture from the Helix Centre, called Digital Care Planning. With NHS funding, it is modernising the way in which ACPs are created and shared within the network surrounding a person living with a life-limiting disease. It does this by genuinely focusing on their individual needs and priorities for care using technology. We learned that some people prefer to quickly establish their priorities of care quickly, whereas others wish to take their time and discuss the details. Surprisingly, we learned that though technology skills vary from people to people, their acceptance of new technologies - voice technology, chatbots - was higher than originally thought. Our approach to technology allows everyone to define their plan according to their own preferences, promoting their autonomy and independence, moving at a pace that is most comfortable.
Our platform, Amber Care Plans is an easy-to-use, free website that captures people’s future care decisions through accessible user interface that is designed for real people, not healthcare professionals. You can learn about all the various aspects of an advance care plan, record your decisions easily, print off for your personal records and digitally share with loved ones. As Gemma, a Marie Curie volunteer remarked, “I’m thinking about my family when filling this out. It’s great to know they have something to guide them.”
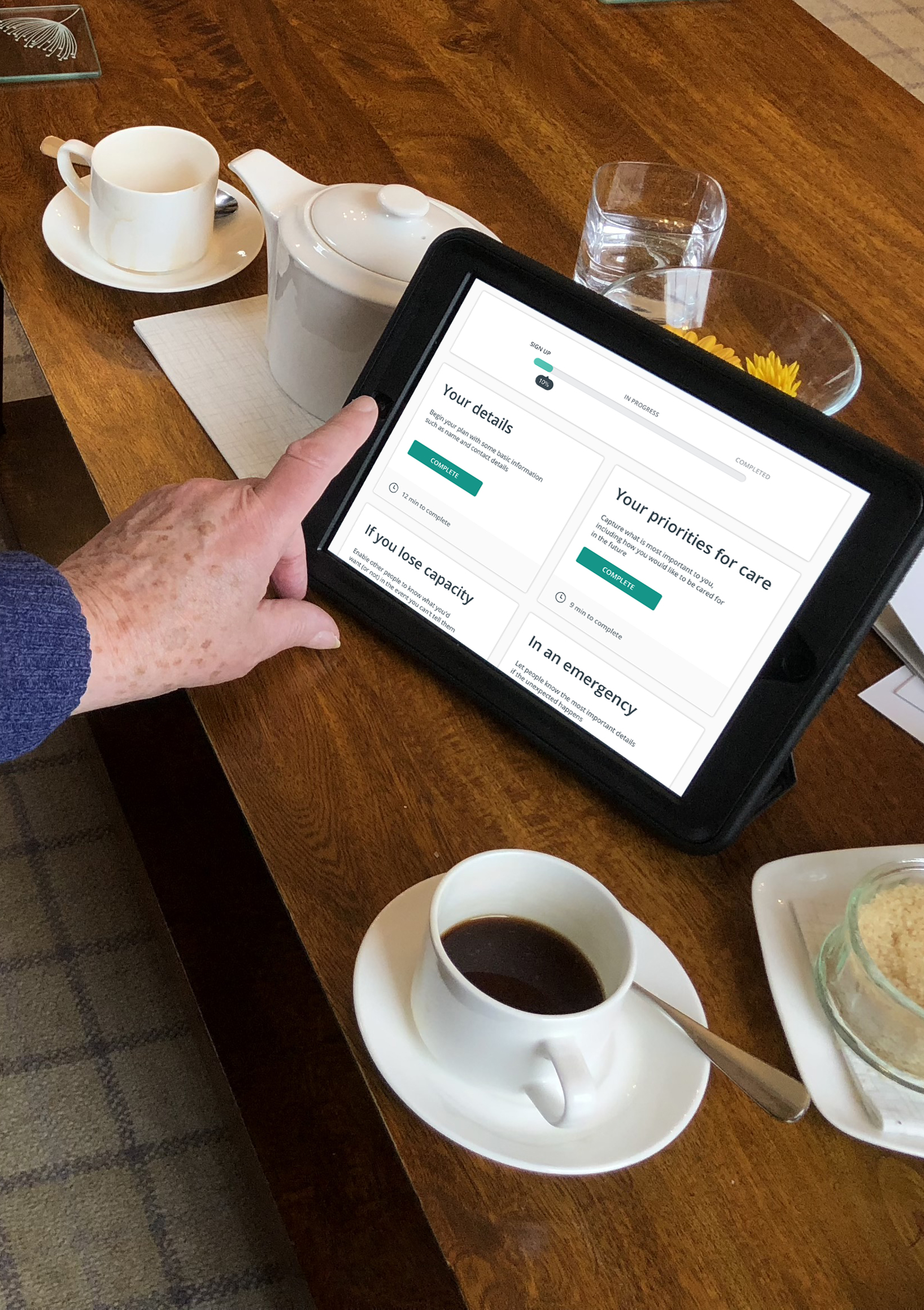
Amber was designed in collaboration with a wide-range of people living with life-limiting conditions
As well as creating a truly person-centred advance care planning tool, we are scaling the ability to create and capture digital care records for the UK health service. Our goal is to effectively and simply connect people with the right healthcare professionals, so that when the time comes, everyone knows what that person wants and needs. The website - amberplans.com - is available for use today, with integration plans in place to connect with NHS services in the near future.
Developing the future of hospice care
The medical innovations of the 20th century radically changed the ways we die, moving it from the home to the hospital, with particular problems we’ve already addressed. In this new century, we need to build a better relationship with death that is open and inclusive, to understand and create better networks, services and places to help us to live well until we die.
It is our mission to define and help deliver future forms of end-of-life care, using contemporary and emerging technologies and practices, and we’re looking at how we can do that with the hospice sector. Hospices perform the most specialised and experienced end-of-life care in the UK, caring for around 360,000 people each year. They are excellent places to meet the many needs of the dying person, however they suffer from a variety of problems, not least of all the fact there are too few referrals from community services and hospitals to hospices which means patients lose out on the experience of hospice staff near the end of their life.
Given many people do not access specialised hospice care, informal carers play a significant role. In any future care model, the needs of these caregivers need to be considered; the caring burden is physical, mental, emotional, and financial, causing high levels of anxiety and stress over a long period of time.
The experience of dying is a deeply human one. It is a uniquely emotional, psychological, spiritual - even mystical - time that everyone will go through. Death can be a terrifying prospect, but good end-of-life care can make a huge amount of difference. We believe that to make radical improvements to the holistic care of the dying person, there is a greater need to support dying people with their psychosocial - spiritual, emotional and psychological - needs. It is vital to not only serve those person’s needs, but broaden the abilities of those caring for them to support and attend to them, both professional and non-professionals.
With the amount of care being delivered by informal - often family - carers, it is vitally important that we both train people to become carers, and support them in being the best carer possible. This can be achieved in the long-term through education, or by identifying the unmet psychosocial care needs and better enabling and equipping people today, to deliver that high level of care.
We have identified five main issues that describe the desire for self-administration of pain relief, the notion of social death, coping with compassion fatigue, accomodation of illness and loss and death anxiety. These issues were factored against six methods to tackle these problems such as peer-to-peer support, training and skills management, new and emerging therapy practices, self-management and others. We are currently developing three new prototype services that tackle some of these complex issues, leveraging the expertise of the hospice movement and the desire for radical change. Patients and families are seeking new tools to support long-term complex needs, to be empowered to care for each other - in their family and in their communities. If done appropriately, technology has a powerful role in enabling this.
By combining human-centred design, relationship-based care models, evaluating and implementing existing and emerging technologies with evidence-based research, we believe we can transform the experience for patients, their loved ones and professionals. We think design can make a huge difference in improving clinical and social outcomes and to the effectiveness of end-of-life care services, particularly for hospices. We are working to establish a tangible vision for the future of end-of-life care, that supports everyone to live as well as possible - with all the joy, sorrow and meaning that comes with it - until the very end.
This editorial was published in the European Journal for Palliative Care in June 2018, in its final edition.